“Where is the wisdom we have lost in knowledge? Where is the knowledge we have lost in information?
—T.S. Eliot, Four Quartets (1943)
Chapter 2: The Breaking Point — When Human Capability Meets Infinite Complexity
A profound paradox lies at the heart of modern oncology. Medicine, once an art guided by intuition and deep human connection, has become an exercise in data management—a profession drowning in its own discoveries. A century ago, great physicians prized knowing the patient with the disease above merely knowing the disease itself. Today, such a distinction feels almost quaint. We have never known so much about disease—its molecular architecture, its genetic signatures, its intricate evolution—yet, paradoxically, we have never been further from the patient who carries it. The very explosion of knowledge that should have made medicine more precise has, in many ways, made it colder, more fragmented, and decidedly less human.
The relentless march of progress has created an unintended consequence – a crisis of complexity that threatens the very heart of medical practice. Consider a moment in the life of a modern oncology clinic. It's 7:15 AM, and the first patient hasn't arrived yet, but the system is already groaning under its weight. Dozens of new clinical trial alerts compete for attention with urgent pharmacy requests about drug shortages. A molecular tumor board report details novel genetic findings in a patient's cancer, each of which requires cross-referencing with rapidly evolving treatment guidelines. Multiple insurance companies require peer-to-peer reviews to justify already standard treatments. The morning's first patient, diagnosed yesterday with pancreatic cancer, arrives carrying printouts about genetic mutations and targeted inhibitors – terms that weren't even part of oncology's lexicon a decade ago.
The numbers alone defy human comprehension. Millions of Americans will receive a cancer diagnosis this year, and thousands of life-altering conversations will take place each day. Behind each statistic lies a human story: a grandmother hoping to see her grandchild graduate, a father wondering how to tell his children, a young woman questioning her fertility preservation options. Each deserves careful attention, but each also requires the integration of rapidly evolving scientific knowledge and an expanding universe of data points that must be tracked, analyzed, and acted upon.
What we are witnessing in oncology might best be compared to the Cambrian explosion, that brief geological moment when life on Earth suddenly diversified into an overwhelming array of new forms. This past decade has witnessed an exponential burst in complexity that challenges human comprehension. Where oncologists once learned a handful of chemotherapy combinations, they now navigate hundreds of targeted therapies, each matched to specific molecular patterns, requiring unique monitoring and carrying their own labyrinthine authorization requirements.
The molecular revolution alone is staggering to the imagination. What was once "lung cancer" has splintered into dozens of distinct entities, each with a different molecular fingerprint, and each demanding unique therapeutic approaches. An alphabet soup of targetable mutations continues to grow more complex by the month. A single patient's tumor genomic report may identify variants in thirty different genes, each potentially significant and requiring interpretation within a rapidly evolving landscape of therapeutic options.
The pace of this evolution defies traditional medical education. In a single year, regulatory agencies may approve more novel cancer therapies than existed during the entire previous decade. Each new approval brings its constellation of biomarkers to test, mechanisms to understand, toxicities to monitor, and resistance patterns to anticipate. The immunotherapy revolution has fundamentally altered our understanding of cancer treatment, introducing entirely new response patterns that often contradict traditional oncologic wisdom. Tumors may appear to grow before they shrink. Conventional response measures no longer apply. The very metrics we use to evaluate treatment success have had to evolve.
Meanwhile, another revolution quietly reshapes clinical practice itself. The electronic medical record, promised as a tool for better communication, has become a frustratingly complex maze of documentation requirements. Consider the simple act of initiating immunotherapy for a cancer patient. What once required a single written order now demands navigation through over a dozen electronic screens. Treatment plans that once fit on a single page now generate forty-page printouts, their essential medical content buried under regulatory requirements and billing codes.
Medicine has reached a tipping point—not from any single change but from the confluence of rapid advancements in science, technology, and economics. The financial complexity alone would bewilder previous generations of physicians. A single dose of modern immunotherapy might cost more than a year's salary for the physician prescribing it. Terms from business administration have become as essential to practice as understanding tumor biology.
These pressures manifest in countless daily moments that erode the doctor-patient relationship. A community oncologist spends her lunch hour on hold with an insurance company, arguing for coverage of a standard-of-care treatment while her meal sits untouched. A young physician updates family members about their mother's condition while simultaneously responding to three urgent patient messages and reviewing laboratory results that continue to populate her inbox. An experienced clinician stays late yet again, spending hours documenting the day's work in precisely the format required for optimal billing, knowing tomorrow will bring the same challenge.
The implementation gap between what we know is possible and what we can deliver grows wider daily. While major cancer centers achieve substantial participation in clinical trials, community practices manage only a small fraction of that. Mortality rates for certain cancers vary dramatically between demographic groups. The disparity reflects not only socioeconomic factors but also the sheer impossibility of delivering optimal care within the current system's constraints.
The human toll becomes increasingly apparent in quiet moments. In break rooms across the country, conversations turn to missed soccer games and postponed vacations, to the growing distance between the medicine we dreamed of practicing and the reality we face. Recent studies have found that a majority of oncologists show signs of professional burnout, while almost a third screen positive for depression. The suicide rate among physicians has climbed to more than double that of the general population, with oncologists facing an exceptionally high risk.
Consider the daily cognitive load: an oncologist seeing twenty patients must track hundreds of discrete data points—laboratory values, imaging findings, medication doses, and toxicity grades—while simultaneously processing new research that might affect each case. Cognitive science suggests the human brain can manage only a handful of information pieces simultaneously. The math doesn't work. One physician noted in a recent perspective that we've built a system requiring superhuman cognitive capabilities, then act surprised when mere humans struggle to operate it.
The triumph of modern oncology—a substantial decline in cancer death rates over the past three decades—has paradoxically contributed to the strain. Millions of cancer survivors now require ongoing monitoring and care. Each survivor requires regular screening, which generates additional data, and each piece of data necessitates human interpretation and subsequent action. The very success celebrated in medical advances has created what might be called "cognitive congestion" in modern clinical practice.
This congestion manifests in subtle and profound ways. A brilliant young oncology fellow trained at a top academic center chooses community practice because the complexity of academic oncology feels unsustainable. A veteran physician retires early, citing not physical fatigue but mental exhaustion from trying to keep pace with the exponential growth in medical knowledge. A promising clinical trial fails to accrue patients not because of scientific flaws but because busy clinicians lack the time to navigate its requirements.
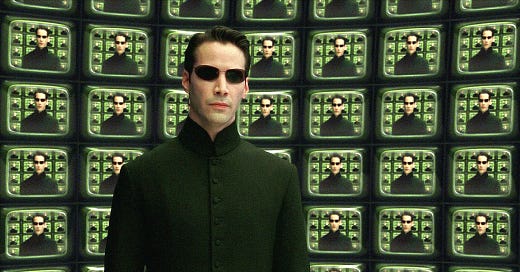
The parallels to another moment in history become increasingly striking. During World War II, at Bletchley Park, a group of mathematicians and linguists faced their own cognitive congestion. The German military was generating more encrypted messages than human codebreakers could possibly process. Each message contained potentially crucial information, each required complex analysis, and each was racing against time. The volume and complexity exceeded human cognitive capabilities in ways that mirror the predicament of modern medicine.
The Enigma machine had created a staggering level of complexity, with possible configurations beyond human comprehension. Today's oncologists face their version of this complexity barrier. A single patient with metastatic cancer can present thousands of data points and potential treatment combinations, each with its evidence base, each requiring integration with that patient's specific molecular profile, comorbidities, and preferences.
The cost of this cognitive overload extends far beyond physician burnout. Each overwhelmed clinician represents hundreds of patients who might miss out on optimal care, not because the knowledge doesn't exist, but because the human mind can only process a limited amount of information. Studies have found that oncologists spend only a few minutes reviewing new clinical trial data per week—a fraction of what would be needed to keep pace with emerging evidence. The gap between what we know and what can be implemented in practice continues to widen daily.
Actual tipping points often become visible only in retrospect. We are all, at heart, gradualists, our expectations set by the steady passage of time. But occasionally, change arrives not gradually but suddenly, fundamentally altering the landscape. Medicine stands at such a moment now. The complexity barrier has become insurmountable through traditional means. Just as the codebreakers at Bletchley Park realized that human intelligence alone could not crack the Enigma, we must acknowledge that human cognition alone cannot manage the complexity of modern medicine. The solution may lie in the same direction those wartime pioneers pointed - not in replacing human intelligence, but in augmenting it. Those early codebreakers demonstrated how mechanical computation could augment human cognitive capabilities without replacing human judgment. Their work also suggests a path forward for medicine.
But first, we must honestly face our current reality. The practice of oncology has reached a breaking point where good intentions, hard work, and human dedication are no longer enough. The cognitive load has exceeded human capacity. The complexity has outpaced our ability to process it. The system demands more than any human mind can deliver.
The ancient physicians who first documented cancer could only observe and describe it; they had no means of treating it. Today's physicians can treat and often cure, but they find themselves overwhelmed by the very complexity of modern care. Tomorrow's physicians may discover, in the marriage of human wisdom and artificial intelligence, a way to finally fulfill the original vision of truly knowing and caring for each patient who has the disease.
As we turn to explore how artificial intelligence emerged from the crucible of Bletchley Park, we must remember what's at stake. This story isn't just about making physicians' lives easier or hospitals more efficient. It's about closing the gap between what we know is possible in cancer care and what we can deliver to each patient. It's about ensuring that the exponential growth in medical knowledge translates into tangible improvements in human lives.





Even though there is an ongoing conversation about the shortages of Healthcare professionals. The impact on the cognitive load and its repercussions on mental health needs serious attention. Thanks Doctor for bringing attention to this issue.