History's Echo: Why We Fear New Tools (Like the Loom)
The Loom, the Luddites, and What they Mean to the Future of Oncology
"Every great advance in science has issued from a new audacity of imagination." — John Dewey
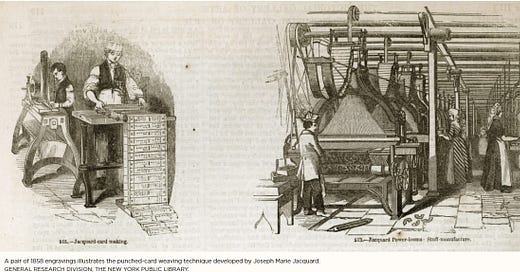
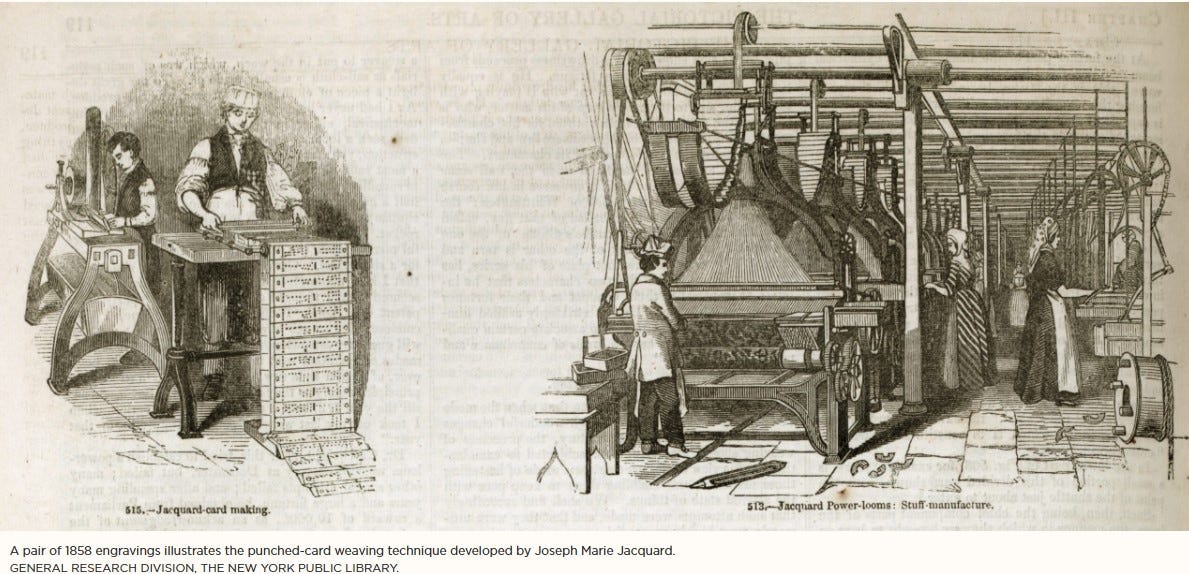
In 1804, a French silk weaver named Joseph Marie Jacquard unveiled a mechanical loom that changed the world—and terrified it at the same time. Jacquard's invention wasn't just an upgrade. It was a revolution. Using a series of punched cards, his loom could automatically weave intricate patterns into textiles—designs that previously required the painstaking effort of master weavers with years of experience.
But instead of celebration, Jacquard's loom sparked panic. Skilled artisans throughout France's silk centers saw this machine not as progress but as a threat to their livelihood and identity. The mechanical loom could produce in hours what took them weeks to create by hand. These weren't people afraid of hard work or resistant to change. These were proud professionals. Craftspeople. Masters whose entire lives were built on a specific kind of excellence and artistic expression. They had invested decades perfecting skills that suddenly seemed at risk of becoming obsolete overnight.
They weren't just fighting change. They were fighting irrelevance. Sound familiar?
The Punch Card That Punched Above Its Weight
Here's what history teaches us—often only in hindsight: That punch card loom didn't destroy creativity. It redefined it. It didn't eliminate human value. It shifted where value lived. Within a generation, France's silk industry had not contracted but expanded. The Jacquard loom dramatically reduced production costs, making what was once an exclusive luxury available to more people. And the role of artisans evolved—from executing patterns to designing them, from physical labor to creative direction.
But Jacquard's influence extended far beyond textiles. Those humble punch cards—with holes representing "yes" and solid spaces representing "no"—embodied a revolutionary concept: stored instructions that could control a machine's operation. This innovation would go on to inspire Charles Babbage's designs for computing machines and Ada Lovelace's visionary ideas about programmable devices. Later, similar punch card systems would help power early IBM computers, becoming a cornerstone of information processing.
It's remarkable to consider that the mechanical loom that once provoked such fear helped lay the foundation for modern computing—and eventually, the artificial intelligence now entering our cancer centers. Innovation, it turns out, often arrives disguised as disruption.
AI in Oncology—Today's Loom(ing) Moment
In oncology, artificial intelligence is having its Jacquard moment. It's new, powerful, widely misunderstood, and for many in the field, deeply unsettling. AI is analyzing diagnostic images with remarkable accuracy, helping to draft clinical documentation, identifying subtle patterns in pathology samples, and synthesizing vast research databases to suggest treatment options. It's doing things we once thought required uniquely human capabilities.
And understandably, many oncology professionals feel a profound sense of unease. Not because they resist progress, but because they care deeply about patient safety, quality of care, and the human dimensions of cancer treatment. In oncology departments worldwide, thoughtful clinicians are raising important questions: What happens to clinical intuition in an algorithm-driven environment? How will trainees develop experienced judgment if machines handle routine cases? What aspects of patient care might be overlooked when treatment becomes increasingly data-driven?
These are not Luddite objections. They're responsible, intelligent concerns from professionals who understand that oncology is as much art as science, as much about healing as about treatment. Because integrating AI into cancer care isn't just a technical challenge. It's a cultural one. It's about trust, transparency, and thoughtful implementation. It's about weaving new technology into the complex tapestry of oncology practice without unraveling the human connections that give that practice meaning.
But just like the loom that once threatened an entire craft tradition, what begins as disruption may become the foundation for a better future—if we approach it with wisdom, intention, and a clear understanding of what technology can and cannot do.
Let's Be Clear—This Is Not About Replacing Oncologists
AI is not here to replace oncologists. It's here to support them. To augment their decision-making. To free up time for deeper human connection, not to substitute for it. We don't need less humanity in cancer care. We need more. What AI can do—when implemented thoughtfully—is help us spend our time where it matters most: with the patient in front of us. It can streamline documentation, support more accurate diagnosis, identify hidden patterns in complex data, and help personalize treatment in ways that no human brain could possibly manage alone across thousands of patients and millions of research papers.
It's not about making oncologists less essential. It's about making them more available for the difficult conversations, the nuanced decisions, and the moments of human connection where technical expertise matters less than presence, empathy, and wisdom.
The Loom Didn't Kill Artistry—It Gave Birth to Design
Here's the part I find most hopeful about the Jacquard analogy: After the loom became widely adopted, something unexpected happened. We didn't lose creativity in textiles. We found new expressions for it. Designers could now experiment with patterns and techniques that were previously impractical. They went from hands-on weavers to visionaries. And the role of the artisan evolved—not diminished, but transformed into something that leveraged uniquely human creativity in new ways.
We're beginning to see similar transformations in oncology. Imagine tumor boards enhanced by AI that pre-analyzes cases and identifies relevant clinical trials; oncology nurses supported by systems that predict which patients are at highest risk for complications; treatment planning that integrates genomic analysis with real-world evidence; and time once spent on documentation and administrative tasks redirected toward patient education, shared decision-making, and emotional support. We're not losing the art of oncology. We're gaining the opportunity to practice it more fully.
Reassurance for the Cautiously Curious
To colleagues who feel cautious about this shift, the concern is warranted. You've trained your entire career to become an expert. You've learned that when it comes to patient care, precision matters. Trust matters. Experience matters. And the idea of algorithms informing treatment plans, analyzing imaging studies, or generating clinical notes can feel like a challenge to professional identity and clinical autonomy.
But here's what's important to remember: AI doesn't replace clinical judgment. It extends your capabilities. You remain the interpreter. The decision-maker. The healer. The human presence. You're still the one sitting eye-to-eye with a patient, translating complex information into understanding, turning fear into hope, and bringing not just expertise but humanity to each encounter. No algorithm can take that from you. And none should try. We're not here to surrender our calling. We're here to enhance it.
So... What Should We Do?
Here's where we get practical. If AI is the loom of our era in oncology, we don't have to wait for others to define its use. We can educate ourselves beyond the hype, learning how these tools actually work, their strengths, and their very real limitations. We can start small with low-risk applications, using AI for draft generation, literature reviews, or pattern detection before moving to more consequential applications. We should demand transparency from developers, ensuring any system influencing patient care is explainable, accountable, and continuously validated.
It's essential that we prioritize ethical implementation, ensuring that AI tools are tested across diverse populations and don't perpetuate existing disparities in cancer care. We must include voices from all oncology disciplines—nurses, pharmacists, social workers, and patient navigators offer crucial perspectives on where AI might help most. Keeping patients informed and involved is non-negotiable; they deserve to know when and how AI is being used in their care. And we need to measure impact rigorously, tracking not just efficiency metrics but effects on patient outcomes, provider wellbeing, and care quality.
The future of oncology isn't about machines replacing clinicians. It's about clinicians empowered by tools that make cancer care more precise, more accessible, and ultimately more human.
The Thread That Ties It Together
So let's return to the Jacquard loom one final time. At first, it looked like the end of an art form. In reality, it was the beginning of a new chapter. What threatened to replace craftsmanship instead became the catalyst for broader access, new creative expressions, and ultimately, technological advances far beyond what anyone could have imagined.
We have that same opportunity now. To embrace this moment of change, not with fear but with vision. To shape AI's role in oncology in ways that honor our commitment to patients while expanding what's possible in cancer care. We don't need to fear the loom. We need to guide its development, influence its implementation, and ensure it serves our highest values—not just efficiency, but equity; not just speed, but safety; not just data, but dignity.
And if we do this right, thread by thread, case by case, we might just weave something better than we've ever seen before. For our patients. For our profession. For the future of cancer care.
Douglas B. Flora, M.D., LSSBB, FACCC
Editor-in-Chief, AI in Precision Oncology
Executive Medical Director, The Yung Family Cancer Center
St. Elizabeth Healthcare